|
|
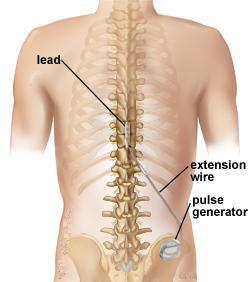
Spinal cord stimulation uses low voltage stimulation of the spinal nerves to block the feeling of pain. It helps you to better manage your pain and potentially decrease the amount of pain medication. It may be an option if you have long-term (chronic) leg or arm pain, and have not found relief through traditional methods. A small battery-powered generator implanted in the body transmits an electrical current to your spinal cord. The result is a tingling sensation instead of pain. By interrupting pain signals, the procedure has shown success in returning some people to a more active lifestyle.
 |
| Figure1 |
What is a spinal cord stimulator?
A Spinal cord stimulator (SCS), also known as a dorsal column stimulator, is a device surgically placed under your skin to send a mild electric current to your spinal cord (Fig. 1). A small wire carries the current from a pulse generator to the nerve fibers of the spinal cord. When turned on, the stimulation feels like a mild tingling in the area where pain is felt. Your pain is reduced because the electrical current interrupts the pain signal from reaching your brain.
Stimulation does not eliminate the source of pain, it simply interferes with the signal to the brain, and so the amount of pain relief varies for each person. Also, some patients find the tingling sensation unpleasant. For these reasons a trial stimulation is performed before the device is permanently implanted. The goal for spinal cord stimulation is a 50-70% reduction in pain. However, even a small amount of pain reduction can be significant if it helps you to perform your daily activities with less pain and reduces the amount of pain medication you take. Stimulation does not work for everyone. If unsuccessful, the implant can be removed and does not damage the spinal cord or nerves.
 |
| Figure2 |
There are many types of stimulation systems. The most common is an internal pulse generator with a battery. A SCS system consists of (Fig. 2):
An implantable pulse generator with battery that creates electrical pulses.
A lead with a number of electrodes (4-16) that delivers electrical pulses to the spinal cord.
An extension wire that connects the pulse generator to the lead.
A hand-held remote control that turns the pulse generator on and off and adjusts the pulses.
The battery inside the pulse generator delivers low voltage and needs to be surgically replaced every 3 to 5 years if it is a standard battery. Rechargeable battery systems may last up to 10 years, depending on usage. Your doctor will select the best type of system for you during the trial stimulation.
The pulse generator is programmable by the doctor and has three settings:
Frequency (rate): number of times stimulation is delivered per second.
Pulse width: determines size of area stimulation will cover.
Pulse amplitude: determines threshold of perception to pain.
Who is a candidate?
Before determining if spinal cord stimulation (SCS) is an option, your condition will be thoroughly evaluated and assessed. A comprehensive evaluation of your pain history will determine if your goals of pain management are appropriate to proceed with treatment.
Because pain also has psychological effects, a psychologist may assess your condition to increase the probability of a successful outcome. A neurosurgeon, pain specialist, or physiatrist will evaluate your current medication regime and physical condition. The doctor will want to review all previous treatments including medication, physical therapy, injections, and surgeries.
Patients selected for this procedure usually have had a disability for more than 12 months and have pain in their lower back and leg (sciatica). They've typically had one or more failed spinal surgeries.
You may be a candidate for SCS if you meet the following criteria:
Conservative therapies have failed
Your source of pain has been verified
You would not benefit from additional surgery
You are not seriously dependent on pain medication or other drugs
You do not have depression or other psychiatric conditions that contribute to your pain
You have no medical conditions that would keep you from undergoing implantation
You have had a successful trial stimulation
An SCS can help lessen chronic pain caused by:
 Chronic leg (sciatica) or arm pain: ongoing, persistent pain caused by degenerative conditions like arthritis or spinal stenosis, or from nerve damage. Chronic leg (sciatica) or arm pain: ongoing, persistent pain caused by degenerative conditions like arthritis or spinal stenosis, or from nerve damage.
 Failed back surgery syndrome: failure of one or more surgeries to control persistent leg pain (sciatica). Failed back surgery syndrome: failure of one or more surgeries to control persistent leg pain (sciatica).
 Complex regional pain syndrome (CRPS): a progressive disease of the nervous system in which patients feel constant chronic burning pain, typically in the foot or the hand. Formerly called reflex sympathetic dystrophy (RSD). Complex regional pain syndrome (CRPS): a progressive disease of the nervous system in which patients feel constant chronic burning pain, typically in the foot or the hand. Formerly called reflex sympathetic dystrophy (RSD).
 Arachnoiditis: painful inflammation and scarring of the meninges (protective layers) of the spinal nerves. Arachnoiditis: painful inflammation and scarring of the meninges (protective layers) of the spinal nerves.
 Other: stump pain, angina, peripheral vascular disease, multiple sclerosis, spinal cord injury. Other: stump pain, angina, peripheral vascular disease, multiple sclerosis, spinal cord injury. |
The surgical decision
Determining whether a spinal cord stimulator will be a good pain management option for you is a complex process. Before a permanent stimulator can be implanted, you must undergo a trial to see if the device decreases your level of pain.
The surgery is performed on an outpatient basis in two stages: Stage 1 is a trial stimulation and Stage 2 is implantation of the permanent device.
 |
| Figure3 |
Stage 1. Trial stimulation
Trial stimulation is very important to determine if the procedure will be successful. It will tell if stimulation is correct for the type, location, and severity of your pain. It will also evaluate the effectiveness of various stimulation settings.
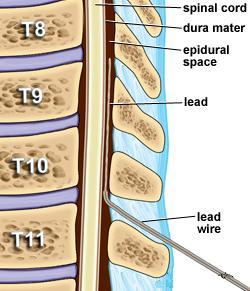
The insertion of a trial lead is typically performed under a local anesthetic. A hollow needle is inserted through the skin (percutaneous) into the epidural space between the bony vertebra and the spinal cord using fluoroscopy (a type of X-ray). The lead is properly positioned and then attached to an external generator and power supply (worn on a belt).
After the trial procedure, you will be sent home with instructions on how to use the trial stimulator and care for your incision site. Keep a written log of the stimulation settings during different activities and the level of pain relief. After 3 to 5 days, you will return to the doctor’s office to discuss permanently implanting the stimulator or removing the trial leads.
Stage 2. Permanent implantation
If the trial is successful and you experienced a greater than 50% improvement in pain, you can be scheduled for surgery. During the trial stimulation, your doctor gathered information about the number of electrodes needed and the type of stimulation that works best for you.
What happens before surgery?
You may be scheduled for presurgical tests (e.g., blood test, electrocardiogram, chest X-ray) several days before surgery. In the doctor’s office, you will sign consent and other forms so that the surgeon knows your medical history (allergies, medicines/vitamins, bleeding history, anesthesia reactions, previous surgeries). Discuss all medications (prescription, over-the-counter, and herbal supplements) you are taking with your health care provider. Some medications need to be continued or stopped the day of surgery.
Stop taking all non-steroidal anti-inflammatory medicines (Naproxen, Aspirin , Ibuprofen etc.) and blood thinners (Coumadin, Plavix, etc.) 1 to 2 weeks before surgery as directed by the doctor. Additionally, stop smoking, chewing tobacco, and drinking alcohol 1 week before and 2 weeks after surgery because these activities can cause bleeding problems. No food or drink is permitted past midnight the night before surgery.
What happens during surgery?
There are two parts to the procedure: placement of the lead in the epidural space of the spinal cord and placement of the pulse generator in the buttock or abdomen. There are five main steps of the procedure, which generally takes 3 to 4 hours.
Step 1. prepare the patient
You are placed lying on your side or on your stomach on the operative table. The team will work with you to make sure you are comfortable before you are given light sedation. Next, the areas of your back and stomach are shaved and prepped where the leads and the generator are to be placed. Local anesthetic will be injected where incisions are to be made to prevent pain during the procedure.
 |
| Figure 4 |
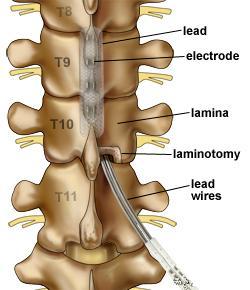
Step 2. place the leads
Placement of the surgical leads is performed with the aid of fluoroscopy (a type of X-ray). A small skin incision is made in the middle of your back (Fig. 3). The bony arch of the vertebra is exposed. A portion of the lamina is removed (laminotomy) to allow room to place the leads. The leads are placed in the epidural space above the spinal cord and secured with sutures (Fig. 4). Your surgeon will decide how many leads and the number of electrodes on the lead to implant.
You will be awakened so that you can help the doctor determine how well the stimulation covers your pain pattern without feeling any pain or discomfort from the lead implantation itself. Your surgeon will decide how many leads and the number of electrodes on the lead to implant.
Step 3. test stimulation
You will be awakened so that you can help the doctor determine how well the stimulation covers your pain pattern without feeling any pain or discomfort from the lead implantation itself. Several stimulation settings will be tried and the surgeon will ask you to describe the location of any tingling you feel. These settings will be used to program the pulse generator at the end of surgery, so your feedback during this part of the surgery is important for providing you the best pain relief.
Step 4. tunnel the extension wire
Once the leads are in place, sedation is again given. An extension wire is passed under the skin from the spine, around your torso to the abdomen or buttock where the generator will be implanted.
Step 5. place the pulse generator
A 4 to 6 inch skin incision is made below the waistline. The surgeon creates a pocket for the generator between the skin and muscle layers. The extension wire is attached to the pulse generator. The generator is then correctly positioned under the skin and sutured to the thick fascia layer overlying the muscles.
Step 6. close the incisions
The two incisions are closed with sutures or staples and a dressing is applied
 |
| Figure 5 |
Discharge instructions
Discomfort
After surgery, pain is managed with narcotic medications. Because narcotic pain pills are addictive, they are used for a limited period (2 to 4 weeks). Their regular use may cause constipation, so drink lots of water and eat high fiber foods. Laxatives (e.g., Dulcolax, Senokot, Milk of Magnesia) may be bought without a prescription. Thereafter, pain is managed with acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) (e.g., aspirin, ibuprofen, naproxen sodium).
Restrictions
Avoid these activities for 6 to 8 weeks to prevent movement of the leads:
 do not bend, twist, stretch, far-reaching, pulling, sudden movement or lift objects over 2.5 Kg s do not bend, twist, stretch, far-reaching, pulling, sudden movement or lift objects over 2.5 Kg s
 do not raise arms above your head do not raise arms above your head
 do not sleep on your stomach do not sleep on your stomach
 do not climb too many stairs or sit for long periods of time do not climb too many stairs or sit for long periods of time
Do not drive for 2 to 4 weeks after surgery or until discussed with your surgeon.
When to Call Your Doctor
If your temperature exceeds 101° F or if the incision begins to separate or show signs of infection, such as redness, swelling, pain, or drainage.
If your headache persists after 48 hours.
If you have sudden severe back pain, sudden onset of leg weakness and spasm, loss of bladder and /or bowel function - this is an emergency - go to a hospital and call your surgeon.
Recovery
Approximately 8 days after the procedure you will come to the office to remove the sutures or staples. Programming of the pulse generator can be adjusted at this time if needed. It is important to work with your doctor to adjust your medications and refine the programming of the stimulator.
What are the results?
The results of spinal cord stimulation depend on strict patient selection, proper surgical technique, intra- and postoperative testing, and patient education. Stimulation does not cure the condition causing pain; it helps patients to tolerate pain. Recent results of spinal cord stimulation show good to excellent long-term relief in 70-80 % of patients suffering from chronic pain .
Living with a stimulator
Once the SCS has been programmed, you are sent home with instructions for regulating the stimulation by controlling the strength and the duration of each stimulation period. Your doctor may alter the pulse width, amplitude and frequencies on follow-up visits if necessary.
The handheld programmer lets you turn the stimulator on and off, select programs, and adjust the strength of the stimulation. Most people are given multiple programs to achieve the best possible pain relief during specific activities. You can use your spinal cord stimulator around the clock if necessary. However, most people get pain relief during the day and turn off the system before bedtime because pain relief often continues even after the stimulation has stopped. Everyone’s pain is different.
Some people feel differences in stimulation intensity depending on their position (e.g., sitting versus standing). This is caused by variations in the spread of electricity as you change positions and is normal. Do not use the stimulator while driving or swimming.
Just like a cardiac pacemaker, other devices such as cellular phones, pagers, microwaves, security doors, and anti theft sensors will not affect your stimulator. Be sure to carry your Implanted Device Identification card when flying, since the device is detected at airport security gates. Department store and airport security gates or theft detectors may cause an increase or decrease in stimulation when you pass through the gate. This sensation is temporary and should not harm your system. However, as a precaution, you should turn off your system before passing through security gates. |
|
|